 Prologue
Prologue
Though less has been mentioned of this particular infectious disease, there leaves a lot to be dwelled on when it comes to mind. Not many healthcare practitioners, especially the more junior ones would have come across it as it is not something overt, such as dengue. The bug’s adroitness in concealment from being discovered leaves much to be frowned upon by senior doctors..
Introduction
So what is melioidosis? Breaking it down to terms – it literally means a resemblance of an equine’s distemper. And no wonder it was called ‘glanders’ back then, though it still is now by the vets. Characterized by swellings below the jaw line coupled with mucoid discharge from the nostrils, this infection is notably due to the similar bug causing melioidosis. Three modes of infection have been described and these are ingestion, inhalation and inoculation (through local wounds). The latter appears to be the most common in our patients.
Cause & Transmission
Melioidosis is caused by a bacterium called Burkholderia pseudomallei. It has an older name which is still used interchangeably by some authorities, and that’s Pseudomonas pseudomallei.
Origins & Ecology
Pseudomallei thrives as a saprophyte- derives its nourishment from dead or decaying organic matter. Both humans and animals aren’t spared either from this notorious bug, which are known to threaten the living daylights out of them.
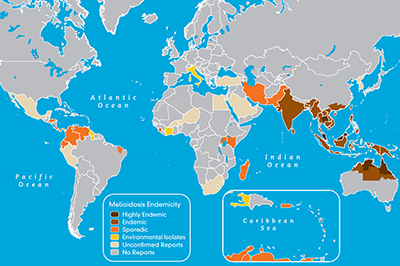
And since they are profoundly innate to the environs of soil, they could be found pretty much around the corners of everywhere, though geographically speaking, the confines of their presence could only be charted predominantly in several countries of South East Asia. A few of these places include Malaysia, Thailand and certain parts of Australia. No doubt literatures that come as references are often cherry-picked by authors from these countries.
Publications have been meager at the start of the 20th century, but it slowly rises over time up to a point of concern where even our Malaysian authorities are frowning their brows over this dreadful infection. Yet, there’s too little that we can do to rid this saprophytic bacterium to extinction. For a start, these bugs love anything and everything that has to do with soil making them omnipresent. The decay that lingers around the earth grants them the opportunity to feed off on any vittles that they can find. Buried deep beneath the soil, they pose no threat to the local populace. It is only with the timing set upon when heavy rainfalls and monsoon periods befalls a certain location that these bugs surfaces to the front and wreak havoc.
Which brings to point, alongside the soil that they are so affectionate of, they too prefer moisture that comes from the damp environment provisioned by nature. Just take a look back at Figure 3 and you will know what I mean.
Characteristics
Now that I have your attention, you would be wondering about the risks involved with regards to contracting the infection. With the enormous possibility of it being everywhere around our soil, and in particular that it peaks during the heavy rainfall season, would you be at risk?
In generality, despite its notoriety, B. pseudomallei appears to be an opportunistic infection. Which brings to mind that if you are fit as a fiddle without any compromising co-morbidity of concomitant illness, such as that of diabetes mellitus, then there’s very little for you to worry about. Put in another better phrase, it’s a big bully of the weakened immune system, but when it comes to a competent challenger, it shies away and scurries off like a mouse. Though even so, literature has recorded cases where patients with competent immune system has been known to be infected as well – the postulation being that they were inoculated with a much greater dose of the bacteria.
Who is At Risk?
Patients with impaired immune system such as those who has:-
- Diabetes Mellitus
- HIV/AIDS
- Kidney failure/kidney stones
- Cancer-stricken patients and/or those who receives chemotherapy
- Patients on long term steroids for certain medical conditions
- Chronic alcohol abuse/dependency
- Local trauma
- Occupational exposure – farmers, rubber tappers
- Natural disasters – floods
Symptoms
Without suspicion, it would literally slip the mind and not be given consideration due to its vague and atypical clinical manifestations. Depending on which organ is affected, the symptoms would localize to that area, though more often than not, patients would complain of prolonged periods of fever, which doesn’t seem to resolve. And these groups of patients would also have one or more of the above risk factors described. When shortlisted as a differential diagnosis, doctors would often enquire upon your occupation, take a detailed account as to whether you may have come across any recent injuries that led to a wound (which might have been healed over the course of time, but the bug may take its time to manifest itself as a full-blown infection).
Despite its vague symptom manifestation, the apogee of melioidosis is ultimately the culmination of abscess or a walled-off pus that could reside in any organ in the body. The lungs appear to be the most common organ involved, but likewise, the liver, spleen, kidneys, brain and prostate aren’t spared either.
Recognition & Treatment
A high index of clinical suspicion remains the cornerstone of nailing the diagnosis followed by blood cultures and radiographic investigations (if necessary) to delineate further the complication that comes with melioidosis (namely, the formation of abscesses). Thankfully, despite its grave implications, treatment with antibiotics is readily available. Though, depending on the presentation and nature of the infection affecting varying individuals, a course of antibiotics is often prolonged, lasting from a decent two weeks course to 4-6 weeks if necessitated. Patients affected are often admitted for that length of time before converting to oral antibiotics for a longer course of between 3-6 months.
Final Words
There’s a saying in one of our local research papers that ‘once a melioidosis, always a melioidosis’ and that’s genuinely unavoidable. Despite the numerous dosages and lengthy duration of treatment administered; the bug remains within, residing, awaiting, plotting and planning to return with a vengeance. Though this statement is somewhat of concern, not all patients succumb to a recurring episode of another melioidosis infection. The risk factors predisposing patients to contracting melioidosis needs to be looked into and addressed appropriately. Occupational exposure needs to be sorted out as well. An introduction of personal protective equipment in the form of rubber gloves and rubber boots prior to going into paddy fields could be an option to consider amongst many.
Thankfully, over time and recognition, melioidosis is now a notifiable disease both in Malaysia and Singapore. Once a blood culture is revealed to be positive, local health authorities demands to be notified within 24 hours.
Dr. Chiam Keng Hoong is a internal medicine physician and a MRCP holder. He currently works in Sabah.
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]
