 When you have a tummy discomfort, passing motion with blood or prolong period of loose stool, you will consult a gastro-enterologist for consultations. At the end of the consultation, you will be advised to undergo a colonoscopy to find out what is the cause of your symptoms. I guess that most of us have face this situation before and wondering whether it is really important to do the test and what is it all about. Is it just another scheme for the doctor to get rich?
When you have a tummy discomfort, passing motion with blood or prolong period of loose stool, you will consult a gastro-enterologist for consultations. At the end of the consultation, you will be advised to undergo a colonoscopy to find out what is the cause of your symptoms. I guess that most of us have face this situation before and wondering whether it is really important to do the test and what is it all about. Is it just another scheme for the doctor to get rich?
What is a colonoscopy?
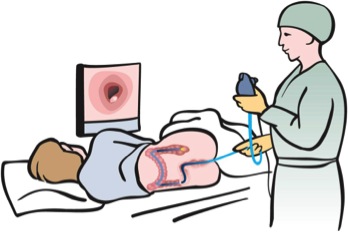
A colonoscopy if a procedure in which a fibre optic cable with a camera mounted at the tip is inserted into the large intestine (colon). The doctor can see in real time what is inside the intestine and determined the diagnosis. If further test / procedure are needed, it can be done at the same sitting.
What is the need (indications) for doing a colonoscopy?
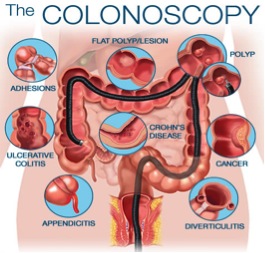
There are many reasons why a patient has to undergo a colonoscopy. If a patient has altered bowel habit symptoms ie – loose stool for prolong period, recent constipations, blood and mucus with stool while passing motion, abdominal pain with palpable swelling in the tummy. All the symptoms suggest that the patient might have cancer of the colon, inflammatory bowel disease or just some small growth in the colon. Hence it is prudent that the patient has a colonoscopy perform so that a definite diagnosis can be made.
What are the things that need to do before undergoing a colonoscopy?
The large intestine (colon) is filled with faeces. The patient needs to clear the faeces before the fibre optic cable can be inserted and have a clear view of the colon. This is call as bowel preparations. The patient is ask not to take any fibre containing diet such as vegetable, meat and protein base diet on the day before procedure. Take only porridge, water, non pulp juices before the bowel cleansing medication. The usual method of cleansing the large intestine is sodium phosphate solution (Fleet®, colclean®), macrogol solution (Fortran®). After drinking the solutions, the patient will start to have bowel motion in about 30 – 60 minutes. The patient is then advice to drink the solution according to the guide. Only when the motion that has been passed contain only watery content and no sediments, than it is considered the bowel is properly cleared and fit to proceed for the scope.
 Will I feel any pain during the procedure? Will I suffer?
Will I feel any pain during the procedure? Will I suffer?
The procedure is fairly common now a day compared to 10 years ago when this medical procedures are still in their infancy stage. With the advancement of the medical instruments, the development of softer and better colonoscope and better training for the doctor to perform the procedure, there will be minimal discomfort. Aided with proper sedative medications given during the procedure, the patient will not feel a thing during the procedure and also cannot remember the entire procedure. At the start of the procedure, the patient is transferred into the endoscopic suite whereby all the necessary medical equipment is there. The patient is put on the endoscopy bed and vital signs monitoring are started. The doctor will give the necessary sedative for the patient to put into a sedated and unconscious mode. Then only the procedure will begin. At the end of the procedure, most of the patient will not be able to recount what went on during the procedure.
What will the doctor do during the procedure?
The procedure, colonoscopy, is basically insertion of the fibre optic cable into the colon. With the help of the camera lens mounted at the tip of the cable, the doctor can see the image on the monitor screen. Under the direct vision, the whole length of the colon can be visualized.
The procedure can be divided in to two types:
Diagnostic – it is just a procedure whereby the doctor will only visualize the entire length of the colon. The doctor will make the diagnosis depending on the finding inside the colon – ie cancer of colon, inflammatory bowel disease, colitis etc.
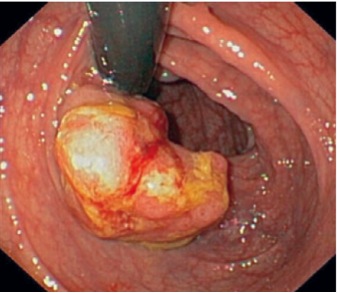
Therapeutic – it an added procedure while performing the diagnostic colonoscopy. When the doctor found a lesion in the colon, ie a colonic polyp. The doctor can, at the same sitting, perform a minor surgery to remove the polyp via the colonoscopy. It is called as polypectomy. Similarly, when the doctor found a growth in the colon and suspicious of cancer, in the same sitting, the doctor can take a biopsy sample of the growth and send it for histopathological examination to confirm cancer of colon.
With the available therapeutic procedure, the early lesion in the colon can be identified and at the same sitting, the lesion can be removed. With this procedure, the patient can have early treatment to prevent the lesion from progressing into a cancer.
 What are the potential hazards / worst case scenarios for the colonoscopy procedure?
What are the potential hazards / worst case scenarios for the colonoscopy procedure?
All procedure carried certain amount of risk for complications. Colonoscopy is the same and cannot avoid complications. In a pair of experienced and safe hands, the risks are quite low.
The complications may be only discomfort in the form of abdominal bloating due to retain air in the colon, pain and abdominal discomfort. These are the minor complications which do not require any interventions. The major risks are bleeding from the colon following trauma from the procedure, perforations of the wall of the colon following any procedure ie – polypectomy, feeling of abdominal bloating due to retain air in the colon, pain and abdominal discomfort. These major complications may need further surgical intervention to manage them. The risk of colonic perforation may range from 0.35% – 2.3%
How frequent should I have a colonoscopy?
The need for a patient to get a colonoscopy is as stated above. After completing the procedure, most of the patient will then ask how frequent should they have the colonoscopy repeated. Most of them are worry that the lesion may grow back. The frequency / duration in which a repeat colonoscopy is recommended depends on the findings/ lesions the patient has in the first place. If the lesion is associated with malignant change (severe dysplasia) from the histopathological report, the patient will be ask to have the scope done once every 6 months to assess whether the lesions has grown back after polypectomy.
If the lesion is benign and have a low risk of cancer, then the repeat scope will be done after 1 year. If the scope findings are normal, the patient could be consider normal up to 3 years if no new symptoms arises.
Colonoscopy procedure is quite a common procedure that is performed in hospital. Due to the evolution and progress of the medical devices, the procedure has increased in safety and efficiency. Largely due to this development, there are even diagnostic centre offering this service to the general public. But one has to bear in mind that all procedure performed on patient carries a certain amount of risks. One need to pick and choose a centre that can offer the procedure and also that can manage the associated complications with colonoscopy. Those centres may be more expensive in the pricing of the procedure but if one need to consider the safety of the procedure rather than cost.
Dr. Lam Yeaw Fah (MBBS, M. Surgery, F.MAS, Dip. MAS, Colorectal Fellowship (SMC, S. Korea)) is a consultant general surgeon and colorectal surgeon working in a private hospital in Klang Valley.
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]
