
Source: www.knowils.info
25th August 2013 : A catch-and-kill attitude was encouraged to be adopted and instilled as the only way to exterminate rats in Kota Kinabalu. A holistic approach with cooperation from local governments and NGOs to tackle the rat problem nationwide included gotong-royong, destroying rat burrows and raising awareness of the local population.
8th October 2013 : Dirty food courts, restaurants and hypermarkets in a commercial area in Kubang Kerian, Kota Baru were identified as providing a favourable environment for rats to populate. Its close proximity to the Universiti Sains Malaysia Hospital was worrying as it was believed that the rats invaded the hospital via underground burrows and sewage pipes linking the two areas.
12th November 2013 : Traders in Yong Peng, Johor highlighted poor hygiene and lacking cleanliness as the main cause for the increasing number of rats and other pests. This led to the Yong Peng district council enforcing a long-term pest control programme to stop the breeding of rats, flies and cockroaches.
March 13th 2014 : The Kuching City North Commission (DBKU) declared a war on rats by doubling its efforts against these pests. One of the suggested techniques was to spray fendona poison inside rubbish bins and eateries, which would cause instantaneous death of the pests coming into direct contact with it.
May 12th 2014 : The Petaling Jaya City Council (MBPJ) stepped up its efforts by launching campaigns to raise awareness on dengue and leptospirosis. Rat poison was set and fogging carried out in a certain neighborhood on that particular day.
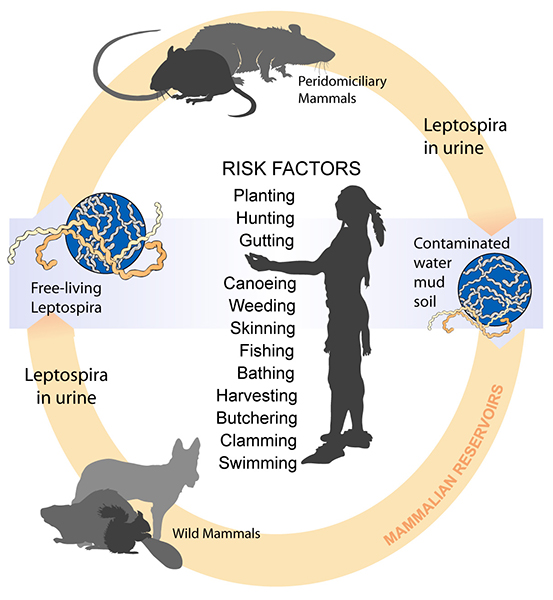
Leptospirosis is commonly known as ‘jangkitan kencing tikus’ or ‘rat-urine disease’. The newspaper excerpts above, are but a few reminders of the effort our local government is putting into exterminating the source of leptospirosis – rats. While the furry abomination is crucial in the spread of the disease, pinpointing the issue to rats itself is inadequate, as there are other hosts such as livestock as well as domestic and wild animals.
From the life cycle, we can see that Leptospira is the bug that causes leptospirosis. Due to its corkscrewed body shape, it is grouped under the category of bacteria known as spirochetes (slender, spiral). These bugs gain entry to the body of both humans and animals through:-
- Cuts and skin abrasions
- Damaged or intact mucous membranes (mouth, nose and eyes)
- Waterlogged skin
- Inhalation of urine droplets or via contaminated drinking water
Upon gaining entry, they are then spread through the body. While humans are accidental hosts and get ill, the real problem lies with infected animals. While they often do not become ill, they continue to spread it to other animals and humans who come into contact with their contaminated urine when they partake in activities such as bathing in still water contaminated with rat urine. Having said that, unhygenic practices as well as dirty and contaminated places are ideal breeding grounds for leptospirosis.
Some of the occupations and activities listed below expose human to a higer than normal risk of acquiring this disease.
| Occupational exposure
|
Recreational exposure | |
| Direct contact with infected animals | Indirect contact |
Walking barefoot in damp conditions Gardening with bare hands Water sports
|
| Farmers VeterinariansAbattoir workers Meat inspectors Rodent control workers |
Sewer workers Miners
Soldiers Septic tank cleaners Fish farmers Gamekeepers Canal workers Rice field workers Taro farmers Sugar cane cutters
|
|
Source: en.wikipedia.org
More often than not, patients who are infected will have a history of exposure to the risk factors mentioned above. Obtaining such history is pertinent in making the diagnosis and thus it would be a great help if patients could recall such related activities in their daily lives.
Symptoms & Complications
The probability of leptospirosis is high in a patient presenting with fever, a history of exposure and two or more of the other symptoms listed below.
- Headache
- Joint ache/soreness
- Muscle ache/soreness
- Red eyes
- Stiff neck, sensitive eyes to light
- Reduced urine output
- Bleeding tendencies
- Irregularities in heart rhythm, heart failure
- Jaundice
- Skin rash
- Nausea, vomiting, abdominal pain and diarrhea
While complications are not common, they may happen in some cases and are worth highlighting for the benefit of awareness. They include bleeding into the lungs, aseptic meningitis, acute renal failure, myocariditis and uveitis.
Management
To confirm the diagnosis and the disease, a blood sample is taken. Management then depends on the extent and severity of the disease. For mild cases, patients may be treated as an outpatient, whereby antibiotics are prescribed and follow-up appointments are given to review symptoms as well as repeated blood investigations. However it should be noted that, if the condition worsens or new symptoms develop, one should consult a doctor for further tests and investigations and an admission may be warranted.
It is recommended that moderate and severe cases are admitted for close and strict observation, so doctors can address any complications that may arise. Furthermore, treatment will include a shift from oral antibiotics towards those given through your veins (intravenously) so as to speed up recovery.
Generally the usual course of antibiotics given is one week, though this does not necessarily translate to a weeks’ stay in the ward, as you will be discharged depending on whether your condition improves or if you develop any complications.
Prevention
As the saying goes “Cleanliness is next to godliness”, thus there is a need to strive for excellence when it comes to the implementation of good hygiene practices and reinforcing hand washing. Food outlets in particular, need to improve their standards of cleanliness and ensure that refuse is discarded properly with screwed on lids which prevent scavengers from crawling in and feeding. Protective equipment such as rubber gloves should be worn when handling contaminated meat as it exposes you to a higher risk of contracting leptospirosis. If frequent hand washing is less than ideal, acquiring a hand sanitizer to be placed in strategic locations in the workplace is another suitable option.
While the government has taken steps to address leptospirosis, it needs to be a collaborative effort between the people and government to properly eradicate the disease. Being aware of these vector-borne diseases and taking the necessary steps as outlined in this article will help in achieving this outcome.
Dr. Chiam Keng Hoong is a internal medicine physician and a MRCP holder. He currently works in Sabah.
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]
References:
- Chan, Z. (2014). DBKU declares war against rats, flies. The Star. [online] Available at: http://www.thestar.com.my/News/Community/2014/03/13/DBKU-declares-war-against-rats-flies-20-major-eateries-in-jurisdiction-identified-for-programme-to-i/ [Accessed 13 Nov. 2014].
- Foo, N. (2014). MBPJ steps up fight against dengue and leptospirosis. The Star. [online] Available at: http://www.thestar.com.my/News/Community/2014/05/12/MBPJ-steps-up-fight-against-dengue-and-leptospirosis/ [Accessed 13 Nov. 2014].
- Lee, S. (2013). Let’s kill rats together. The Star. [online] Available at: http://‘Let’s kill rats together’ [Accessed 13 Nov. 2014].
- The Star, (2013). Pest breeding grounds too close for comfort. [online] Available at: http://www.thestar.com.my/News/Nation/2013/10/08/Pest-breeding-grounds-too-close-for-comfort/ [Accessed 13 Nov. 2014].
- The Star, (2013). Campaign to fight against rats invasion in Ayer Hitam. [online] Available at: http://www.thestar.com.my/News/Community/2013/11/12/Campaign-to-fight-against-rats-invasion-in-Ayer-Hitam/ [Accessed 13 Nov. 2014].
