In continuation with previous article, I will further discuss on investigation & management of Nasopharyngeal Carcinoma (NPC)
After history & clinical examination, next step is confirmation of diagnosis. Decades ago, ENT specialists depend solely on use of posterior rhinoscopy. This is by use of tiny mirror, attached at a 45 degree angle to a slim metal which is inserted to the mouth. With good lighting, it offers a view of the furthest corridor of the nose where the cancer lies. Fortunately, with advent of endoscopy, we now have a wide angle view of the nasopharynx with minimal discomfort to the patient. With camera attachment- the images can be viewed by the patient & relatives for better understanding of the disease.
Next step is the biopsy, which is tissue sampling of the growth, which is the confirmation of the disease. With endoscopy and local anaesthesia, a slim metal forceps is inserted into the nostril and tiny piece of the tumour is wedged off. This is done as outpatient as the pain ranges from very slight discomfort to moderate pain in few subjects. It will cause slight bleeding but extremely rare needing admission. This is a huge advantage of endoscopy, comparatively to the olden days where admission to ward is needed because patients needed to be general anaesthesia as access to nasopharynx is similar to doing adenotonsillectomy.
Fortunately in my centre, our biopsy result from the Pathology Department comes back as early as 3 working days for urgent cancer specimens. This has tremendously helped us in speeding up patient’s treatment.
Breaking bad news in our setting can be very time consuming or very fast. The educated demanding patients will ask many questions from head to toe & may have emotional breakdown at times. The not so educated ones sometimes have no idea what we explain and sometimes even smile when we tell them- “you have cancer”, because they have no idea what hit them. At end of our lengthy explanation in the most layman term, some will say- “we leave it up to you doctors, because you know what’s best for us”. The good thing is- they will accept our treatment. The bad thing is- they do not know what they are getting into.
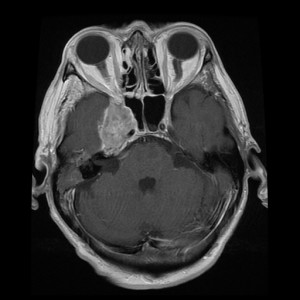
Next is staging of the disease, mainly by Computed Tomography (CT) scanning. In our hospital, we prefer to have the scan done from skull base down to the abdomen, to assess extent of the disease. Previously, our practice was CT neck, with chest plain radiograph (X-ray) and ultrasound of the liver. However, there were many instances, the distant metastasis were missed. We are also fortunate that our CT scan appointments are given rather early in cancer cases, given many other cases from other disciplines who share the use of the same machine.
The patient will also undergo basic bloodwork such as full blood count, serum electrolytes, liver function test and Hepatitis screen prior to treatment. We also need to look into any pre-existing medical illness such as kidney disease, stroke, heart disease which may interact with chemotherapy agents.
Finally, patient will be offered for treatment. This will be largely managed by my Oncology colleague in our new Likas Nuclear & Radiotherapy Centre. We run weekly clinic discussing treatment options for new, on going and ones completed treatment, for cancer of nasopharynx and other head & neck cancers. We also deal with complications of treatment & diseases.
Main modality is radiotherapy- which is by mean of ionizing radiation delivered via external beam at tumour site. Some doctors describe radiotherapy as ‘current’, as in electricity, to the patients. Small percentage will fled for their lives in view of the horror of being electrocuted if they don’t ask further elaboration of treatment. Radiotherapy will be given usually over a period of an average 35 fractions or sessions lasting about 7 weeks.
Chemotherapy is part of treatment. It may be given initially for huge tumours, to shrink the tumour bulk which will later be more suitable for radiotherapy to act. The patients will be warded about a week, with subsequent 2 weeks break- this constitutes a cycle. Up to 3 cycles can be given. Small doses of chemotherapy will also be given every week midway through radiotherapy to enhance the tumour killing effect of radiotherapy.
Surgery is reserved only for recurrent cases & residual tumours. It depends on the site as well- whether for neck dissection for neck node recurrence or excision of small nasopharyngeal tumour via endoscopy for local recurrence.
Some of our patients are from far, so they will be in ward throughout the treatment, with breaks over the weekends. Some defer treatment on hearing 7 weeks admission fearing that no one can support the family, mainly if they are the sole breadwinner. Minority defaulted treatment halfway as they are unable to come back for treatment in view of financial reason. Few have dropped out of treatment as they felt better halfway through, only to come back months later with advanced disease.
In incurable cases, recurrence of tumour which cannot be salvaged and if patient refuse any form of treatment- we offer palliative care. We are blessed to have an awesome Palliative Care team, which was established way before many other states in Malaysia. They offer all services- medication, nursing care, support groups, spiritual advices, relaxing activities among many. What else is more to be offered than for a person to die with comfort and dignity?
In next & final part, I hope to discuss the issues related to patient and physician reaction in handling the cancer.
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]