
Source: www.advancedhealthcareforwomen.info
Laughter is the best medicine but not when you have ‘leaky pipes’. Imagine this: You gather with a group of friends to reminisce about the good old times. You howl in laughter over some funny story your friend just shared and the next thing you know, you’re rushing to the ladies room because things are a little wet down there.
Another similarly embarrassing scenario: You receive a bouquet of flowers from the love of your life, a token of your 10th anniversary together. You deeply inhale the scent of the white calla lilies. What should be followed by a contented sigh was instead followed by a big sneeze (well, you somehow forgot that you’re a little sensitive to flowers, but hey, who could resist big, beautiful bouquet of flowers?). Not wanting to abandon your man there and then, you just cross your legs and try to hold it in a little bit more, counting the seconds when you can gracefully head off to change your underwear.
Sounds familiar? Well, for those who have no idea of what is happening in these two scenarios, let me tell you this. Women are sometimes riddled by the misfortune of having urinary incontinence (UI), a condition whereby for some reason, she experiences uncontrolled leakage of urine. It is an unintentional condition that is common but nonetheless distressing. It may be a small matter to some, but to others, it is a problem of epic proportions. So much so, that there is even a global society especially dedicated to it. The International Continence Society defines urinary incontinence as being ‘the complaint of any involuntary leakage of urine’. Innocent and mindless acts of laughter, coughing or sneezing may trigger the incontinence. The good news is, it is fairly treatable and preventable.
So, all UI is the same, right?
Nope. Basically, there are different types of urinary incontinence, simplified as follow:
- Stress incontinence: This type of incontinence usually occurs when there is exertion or effort involved, for example, sneezing or coughing. The muscles involved in supporting the urinary bladder and its mechanical functions are weakened. The sphincter, or the gatekeeper so to speak, is unable to contain the urine in. Normally, the bladder is pretty hardy and can withstand just about any pressure, but in UI, when there is a sudden increase of pressure, the sphincter just fails.
- Urge incontinence: This condition occurs when there is involuntary leakage of urine just as someone gets the urge to urinate. In other words, one simply cannot hold it in, in time to make it to the loo.
- Mixed incontinence: This is a mixture of both urgency and stress incontinence. Not only the sufferer involuntarily leaks urine when the urge comes, but she is also afflicted by incontinence when there is any form of exertion involved, such as coughing or sneezing.
- Overactive bladder: An overactive bladder may or may not occur with urge incontinence. However, it is associated with an increase frequency of urinating as well as urinating at night. Hence the name.
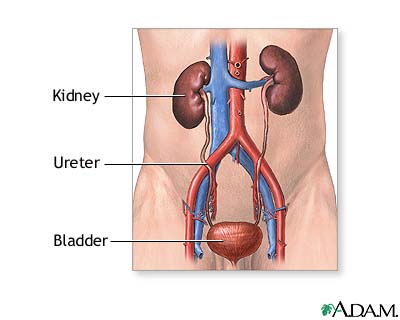
Source: A.D.A.M Interactive anatomy
Tell me what this whole urinating business is about…
Before we continue our excursion, let me just explain the basic mechanism of urinating. Our kidneys produce urine continuously. They work hard to ensure that our body gets rid of any waste. From the kidney, the urine trickles down to the bladder, which is basically a retention room for the urine whilst waiting time to be deployed. It is made up of muscles and can expand according to how much urine is collected. The outlet for the urine is the urethra, which is normally kept closed. This involves teamwork whereby the pelvic floor muscles assist in keeping the gateway closed by giving support around the urethra. When the urge comes, the bladder will contract and the urethra and pelvic floor muscles will relax to allow the urine to flow out. There are other complex nerve messages involved as well, so not only does this involve the players mentioned above, but it also involves the almighty brain.
Now that the mechanics are clear, it is easy to see where and what could go wrong and subsequently result in incontinence. Women, in general, are more prone to be affected by UI. In fact, it is twice as likely to occur in women rather than in men, due to the difference in the structure of the urinary organs. Top that off with the injury and weakness of muscles involved especially during pregnancy and childbirth, and you’ve got the perfect recipe for developing UI. Older women are more predispose to UI than younger women. But putting all that aside, other reasons can also cause UI, such as nerve injury, stroke and birth defects. So basically, UI happens when there are problems with the muscles and nerves that help hold or release the urine.
How would I be checked for UI?
Of course, the first step to relief this problem (no pun intended) is to see a doctor, who will go through the process of asking about your symptoms, medical history, and other relevant questions. You would probably be asked to keep a weeklong diary, describing your voiding in detail. Incidences of urinary leakages and activities associated with it would also be crucial. Usually, this diary would reveal the nature of your UI and the doctor would then have narrowed down the cause of your UI.
He or she would then proceed with doing the necessary investigations. A thorough physical examination would be carried out, and this may include examination of the vagina or the birth canal for any prolapse (where the vagina or bladder protrudes out of the body), which is also a common cause of UI. This is followed by relevant tests that may include blood tests, urine tests and ultrasound scan. Your doctor may order other tests based on individual needs.
Let’s sort out this problem…
UI is a treatable condition. Full stop. And the treatment options vary based on the root of the problem. Someone who has an overactive bladder may need certain medicine to overcome the problem. Vaginal or bladder prolapse may require surgical correction, but it can also be resolved by a simple device into the vagina to give support to the surrounding walls.
Most of the time, for UI caused by muscle weakness, ‘retraining’ of the bladder may be all that is necessary. This involves going to the loo at a timed interval, which simply means setting specific time to void. Once you are used to this, the time interval may be set a bit longer than the one you started off with. This technique does not guarantee overnight success but with time, you may be able to show your bladder who’s the boss.
On top of this bladder retraining technique, you will need to strengthen your muscles down there. The combination of these two techniques will ensure greater success of bladder control. This requires you to perform the Kegel exercise religiously. This, too, is not something that can be achieved at a blink of an eye, but rather requires ongoing practice.
Source: www.brighamandwomens.org
Kegel Exercise
To do this exercise, you need to find the right muscles. Imagine you are trying to stop urine flow or trying to stop yourself from farting (passing gas). Try doing it but don’t involve your abdomen, legs or buttocks. That is your pelvic muscles.
Once you are familiar with this group of muscles, all you need to do is squeeze them in, hold for 2-3 seconds, then release. Repeat the process for 10 times, and then relax. This is considered as one complete set. Try doing it for three sets. The best way to start doing this is by finding a comfortable spot, where you can concentrate without external disturbances. Some may want to start by doing the exercise lying down, and then as you progress, do it sitting up. But my advice is to be patient. Although it only takes about 5 humble minutes of your whole day, its impact will be very fruitful.
On a parting note, let it be clear that urinary incontinence is a common problem, but it is still a bothersome problem. The good news is that it is very much treatable and in some cases, preventable. All it takes is your own awareness (which is what I hope to achieve by this article) and the patience to work with your doctor to overcome this situation.
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]
Dr. Ayu Akida is a Public Health specialist. Her area of interest is family health, especially women’s health and infectious diseases. Find out more about her at The Team (Columnist) page.
References:
- Urinary Incontinence In Women, National Institutes of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health & Human Services.
- International Continence Society

I have this problem 🙁