Imagine this: you open your eyes and see a bright light. You see figures moving in front of you but you have no idea what is happening. Suddenly you feel hands on your body and turn you to the left. They are doing something to you but you do not know what. You close your eyes.
Tick. Tock. Tick. Tock. Time passed by without anyone realizing it.
Three months later: you open your eyes and see the light again. You still do not know what is happening. You see figures in white moving in front of you. And you see a familiar face. Without realising it, you feel warmth on your cheek and you know you were in tears. You hear “Look, he is crying. It has been a while for me to see your blank face without reaction.” Listening to this, you still do not know what had happened, and why you are crying. And again you feel hands all over you and you feel that you are being turned to one side. They did something to you but you still do not know what is happening. You close your eyes again.
The above is a description of the feelings of a person who is alive but in a certain state. A state in which the person is awake but not really conscious. He, or she, will not be able to respond to his or her surroundings. The vegetative state, as you might guess, is a condition that renders a person to become like a vegetable. Staying in one place without any purposeful movement until someone comes and moves you. You are helpless, but surrounding people will help you with activities of daily living, such as toileting and grooming. You will also be fed regularly as you are unable to do it yourself.
Have we ever encountered these scenarios? What do we understand of this term “vegetative state”?
Scenario one: One fine day a family member of a severe traumatic brain injury patient commented to the doctor; “Oh! (gasp) he is looking at me and crying. But when I talked to him, there was no response. Even when I pinch him, he did not react. What does this mean doc? Is he comatose? Or is he a ‘vegetable’?”
Scenario two: One young woman sustained a cardiac arrest (heart stopped beating) for a significant time and subsequently developed hypoxic brain damage secondary to lack of oxygen reaching her brain. She survived the condition and had been in persistent vegetative state for many months. She is depending on her caregiver for her feedings and her other activities of daily living. Will she improve further? Will she return to her condition before the cardiac event? Should we stop her ventilator support, or feeding in that sense? Will she die because of improper care?
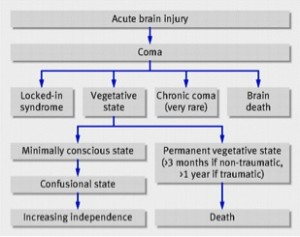
I would like to bring this topic into light as we might be confused with many other terms that may sound similar but are are, in fact, different. You might have heard these words: (i) coma, (ii) vegetative state, (iii) persistent vegetative state, (iv) permanent vegetative state and (v) brain death. In this article, I would like to emphasize on the persistent vegetative state.
 One thing that we can agree upon is that these words or sentences must have something to do with the brain. The brain got damaged in one way or another, so it does not function the way it should. As a person, we should be able to do a lot of things in a purposeful manner to complete all the activities of daily living. Examples of these activities are toileting and eating. Not only that, life sustaining processes such as breathing and beating of the heart should take place without our realisation. Most importantly, a normal functioning brain will be able to make a person aware of his surroundings and react to them, and able to be aroused at any time or stimuli, or in short wakefulness.
One thing that we can agree upon is that these words or sentences must have something to do with the brain. The brain got damaged in one way or another, so it does not function the way it should. As a person, we should be able to do a lot of things in a purposeful manner to complete all the activities of daily living. Examples of these activities are toileting and eating. Not only that, life sustaining processes such as breathing and beating of the heart should take place without our realisation. Most importantly, a normal functioning brain will be able to make a person aware of his surroundings and react to them, and able to be aroused at any time or stimuli, or in short wakefulness.
Even though the brain sits within a hard structure, namely the skull, it can still be damaged from various reasons. The commonest mechanism of injury to the brain would be trauma. It is quite prevalent in our country as mentioned in the National Trauma Database (NTrD), which is a group of local experts who sit down together in order to get local data so that we have clearer pictures of the demographic of traumatic brain injury in Malaysia. The initiative was started in 2003.
Other causes of brain injury would be infection (e.g. meningitis) and bleeding (e.g. haemorrhagic stroke or aneurysm rupture). Those causes need a specific kind of treatment from the treating doctor at various centres. Diagnosis has to be established carefully before administering the treatment in order to optimise recovery from the damage to the brain. These patients need long term care so that they can recover. In other words, the patients need rehabilitation after receiving the treatment for their conditions.
The vegetative state is a condition in which patients has a disorder of consciousness. This condition has been described by Jennett and Plum in 1972. The state is characterized by ‘wakefulness without awareness’. The patients appear to be awake and can be aroused by painful or salient stimuli. They appear to regain back the cycles of opening and closing their eyes, resembling sleep-wake cycles but whether it is actually reflecting the circadian rhythm (day-night rhythm) in a normal person is questionable. They may make movement but do not interact with others and make no purposeful or voluntary responses to visual, auditory, tactile or noxious stimuli. They show no ambiguous signs of conscious perception or deliberate action, including communicating acts. Basically we see a person, who is either bedridden or wheelchair bound, recovering from any type of injury to the brain making movements but is neither reacting nor connecting to the surroundings. The movements they make are without any purpose. They may be clenching their fist, or grimacing to a certain sounds, or chewing without food in their mouth. Even though they make movement and sounds, they do not respond to threatening gestures or able to have consistent and reproducible visual fixation. The patient cannot, or will not react to the situations, which in a normal person would perceive as threatening. They just wait and receive any noxious stimuli presented to them. The patients also have no control over their bowel and bladder (incontinence). The caregiver needs to help with their activities of daily living.
How long does this vegetative last in the patient? Shortest version of a long answer, I don’t know.
When the condition of the patient is prolonged for more than a month, they would be termed as being in a “persistent vegetative state”. During this time, the patient needs assistance in order to live for another day. They need help and the patient might recover, which quite often occurs in patients of a younger age and when the cause in traumatic. That is why the role of caregiver, regardless either one of the family members or trained personnel, is quite important. They have to do two things to get by each day:- one for themselves and the other for the patient. It is a very tiring job for a person to handle. You need all the help you can get to deliver the care. It is a repetitive task as days goes by. The repetition may be taxing for some after a period of time. The caregiver just has to bear in their mind that, the persistent vegetative state patient needs someone who will be patient for their recovery. And the road to recovery is often a long one.
As a bystander it is relatively easy for me to say, “you have to help the patient with rehabilitation so that he or she will improve”, as compared to the one who is delivering the care. One thing that is so crucial during this persistent vegetative state is that, if the care delivery is stopped, the patient may die long before he or she recovers. The potential for recovery will be thrown down the drain if care is put on hold at any time. Pneumonia, bedsores or urinary tract infection, to name a few conditions, can kill the mishandled patient who is in the persistent vegetative state. The second scenario illustrates that there are lots of legal problems and discussion as this kind of patient takes up too much resources, mostly felt by the caregiver. You will find various reasons to continue or discontinue health care in such patients. One of the popular reasoning for cessation of care is that the patient is taking up too much resources, which is an injustice to others, who may have better prognosis or outcome. Frankly speaking, it is really up to the caregiver or the loved ones who will render the effort in order to deliver the tender and loving care.
After more than a year and recovery is at a static point, then the patient is said to now be in the “permanent vegetative state”. Time limit is slightly limited in non-trauma persistent vegetative state. Their status will be changed to permanence when recovery after 3 months seems unlikely.
I will end this article by saying “In dealing with persistent vegetative state, it is important to keep in mind that it is a difficult time for both the patient and the caregiver.”
Dr. Rahmat is a neurosurgeon who believes strongly that knowledge empowers the public to make the right choices. Read more about him at The Team page.
References
- Martin M Monti, Steven Laureys, Adrian M Owen. The Vegetative State: Clinical Review. BMJ 2010;341:c3765
- Adam Zeman. Consciousness. Oxford University Press 2001. page1272
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]


Hi! Dr,
My aunt (aged 54+) is in similar condition of Scenario 2 but have not reached the persistent vegetative state. She’s still in ICU & has been unconscious for a week now.
1) Is there a chance for her to be conscious again / live / wake-up?
2) What should we do to increase the possibility of her being conscious again?
3) Does she still have hope?