Source: www.webmd.com
Currently, there are two ways to investigate women’s reproductive system using ultrasound. One can find these two methods in almost all clinics or hospitals providing obstetrics and gynaecological services. If patients come for consultation and they need ultrasound scans, the sonographers or radiographers will do the transabdominal and, if need be, transvaginal scanning procedures.
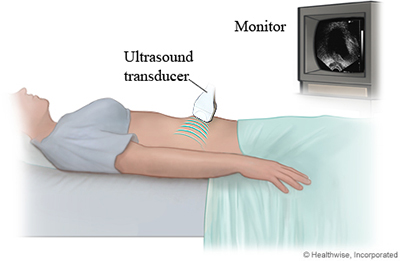
Transabdominal scan (TAS) is usually the initial scanning procedure to be done. It is a non-invasive procedure and more commonly found in health establishments. Since it is only done on the exterior, diagnosticians have more space and more area to operate and manoeuvre the probe. And since it is non-invasive, it is suitable for both married women and women with no prior intimate interaction.
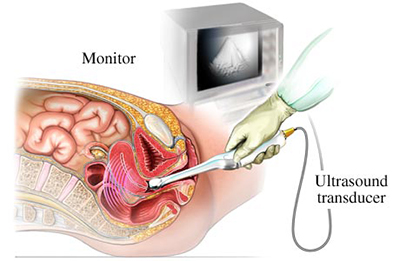
Transvaginal scan (TVS), however, is less common. This is due to the fact that to operate a TVS probe, one needs proper training to orientate the tight space. It is invasive as the probe needs to be inserted into the vaginal orifice. Unmarried, single or ladies with no prior sexual intercourse are seldom offered this option.
TAS can offer a wide angle image but sometimes, the imaging has its limitations. To obtain a good image, the patient’s bladder needs to be full. The bladder will act as a ‘lens’, and ‘intensify’ the sound wave passing through the uterus. Thus, at times, the patient needs to hold their bladder (not urinate prior to the test) and this leads to slight discomfort. And since sound wave imaging is influenced by distance and materials the wave have to pass through, imaging obese patients or patients with retroverted uterus (uterus angled to the back) will yield somewhat unsatisfactory pictures.
Source: www.fssc.com.au
This is where TVS comes into play. The TVS probe, which enters the vaginal orifice can get closer to the organ and obtain a clearer image. The sound wave can now bypass unwanted tissue (skin, abdominal fat, intestines) and get directly to the organ of interest. The only problem now is the limited range of movement. TVS can visualise ‘hidden’ ovaries, ectopia, small gestation sacs and sometimes early fetal heart activity. A closer distance means eliminating the resolution errors, sharper image and more accurate measurement.
In either case, the patient will never be alone with the sonographer. There must always be a nurse as a chaperone to fulfil the ethical requirement. I, myself as a male sonographer, will try to keep the patient’s privacy and allow the nurse to assist me to insert the TVS probe.
Azizul Ismie is an Australasian Society of Ultrasound Medicine (ASUM) certified sonographer working in a maternity clinic in Kuantan.
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]
Reference:
- Diagnostic Ultrasound, Rumack, Wilson, Charboneau.
- Applied physics and technology of diagnostic ultrasound, Gent.
